Introduction
The sterile hold time depends on the sterilization wrapping system, operator performance and sterilization cycle performance. After sterilization occurs, parts and equipment are to be used within a timeframe that is tested and validated. This allowable hold time is established for each sterilized item and associated sterilization wrapping system and is generally confirmed by an aseptic process simulation (APS). Benchmarking was completed of manufacturers within the pharma and biopharma industry to determine if common practices exist for establishing hold times for autoclaved items used within aseptic fill/finish manufacturing.
Established hold time is confirmed by using “expired” parts installed on the filling line or in aseptic filling operations as part of the routine APS. Using sterilized parts at the end of the hold time in the APS confirms the parts remain sterile through the expiry period. The hold time studies allow for sterile parts storage, thereby eliminating the need to sterilize materials the same day as the filling process.
For items required to be sterile, sterilization wrapping (bags and pouches) allows for steam penetration during autoclaving and maintains a microbial barrier post sterilization. The wrapping allows for parts and equipment to be moved throughout the facility and within the clean rooms without compromising the critical product contacting surfaces. Double wrapping or using a wrapping material that is compatible with manual application of surface disinfectants are both recommended methods of reducing risk during material transfer into higher classified spaces. For these reasons, defining the sterilization wrapping system (material of construction and closure method) is essential.
To test and confirm sterilization wrapping system performance, studies7 have been conducted using various bags, pouches, and closure methods over a defined hold time of 30 days. Biological indicators were used to confirm sterilization at time zero and sterility testing was performed throughout the hold time duration.
Regulatory Requirements and Industry Guidance
Multiple regulatory (FDA, MHRA, HPRA, ANVISA, EMA) agencies discuss the need for hold time studies to be completed to support parenteral drug manufacturing. With regards to the packaging, this is defined in more detail in the newly released EudraLex: Volume 4, Annex 1 and addressed in other regulatory guidance documents. There are also industry guidelines that discuss using sterile held parts within the APS.
European Union EudraLex: Volume 4, Annex 11
- 46: “Where possible, materials, equipment and components should be sterilised by validated methods appropriate to the specific material. Suitable protection after sterilisation should be provided to prevent recontamination. If sterilised items are not used immediately after sterilisation, these should be stored using appropriately sealed packaging. A maximum hold time should also be established.”
- 48: Where materials, equipment, components, and ancillary items are sterilised in sealed packaging or containers, the packaging should be qualified for minimizing the risk of particulate, microbial, endotoxin/pyrogen or chemical contamination, and for compatibility with the selected sterilisation method. The packaging sealing process should be validated. The validation should consider the integrity of the sterile protective barrier system and the maximum hold time before sterilisation and maximum shelf life assigned to the sterilised items. The integrity of the sterile protective barrier system for each of the sterilised items should be checked prior to use.
With the increased level of detail provided in Annex 1, some expectations are much clearer, but there are some expectations where the execution methods are not explained. Annex 1 now specifically says that hold time studies are required, but how to perform this testing is not explained.
USP 12112: Equipment in direct contact with components, containers, closures, and sterile products
- The procedures used for the cleaning and sterilization of direct contact surfaces, including dirty, clean, and sterile hold times, must be validated to ensure they do not adversely impact essential product quality attributes as well as to verify the effectiveness of the cleaning procedure and that no microbial recontamination/proliferation occurs during equipment storage.
Parenteral Drug Association (PDA) provides the following guidance to the industry in Technical Report #22, “Process Simulation for Aseptically Filled Products”5 . In this section, the information is describing worst case examples for developing the APS.
- 3.2… Other examples of “worst-case” practices may include: Using room/equipment at the maximum time period after completion of sanitization/ sterilization (clean hold time).
Regulatory and APS considerations are discussed in Pharmaceutical Engineering March/April 20224 when developing the simulation to meet all of the needs of the process. The list below contains examples of some of the worst-case challenges that are expected to be carried out within an APS.
- Page 51: APS Considerations- Worst Case Challenge:…
- Hold Time
- Equipment/room clean hold time
- Equipment sterilization hold time
- Hold Time
Operational Advantage
Hold time testing ensures package integrity to protect the sterile part or equipment. Packages can then be held in a cleanroom post sterilization and can be ready to use when needed without extra preparation time. The autoclave is in high demand in most facilities and the extra reprocessing time is costly and just in time availability may be limited. Confirming a hold time also allows for less reprocessing of autoclaved parts/equipment if not used within production on the same day as sterilization.
Decoupling the sterile hold time from the APS reduces the possible variables if a failure occurs. Because of the worst-case scenarios tested, removing any unnecessary variables allows for a more streamlined investigation and root cause determination.
Re-qualification
As mentioned previously, a sterile hold time would be confirmed during an APS. Use of expired material would be re-qualified during this testing. However, the APS purpose is not only to confirm a sterile hold time. Within an APS, there are multiple variables all being tested as the worst-case process. Because of the multiple variables, determining the root cause of a failure is difficult. Separating the sterile hold time studies and the APS reduces the variables during the simulation. If this decoupling does not occur, it would be difficult to pinpoint the sterile held parts as a root cause in the event of a failing simulation.
Designing Experiments
Sterility assurance is maximized by confirming hold times of parts or equipment used for aseptic manufacturing. Each end user is required to validate routine wrapping configurations using representative parts and equipment for a time range that fits the individual process. This wrapping should be easy to reproduce for employees to ensure consistency. The consistency of wrapping can help confirm the microbial barrier is intact after each sterilization cycle. The sterile hold time should be confirmed by the end-user and tested during an APS.
During a hold time study, there are multiple variables that are needed to be tested to create a comprehensive study. Some examples that were benchmarked from the biopharmaceutical industry are listed in table 1 below.
| Variable | Example |
| Duration | 30 Days |
| Part | Stopper Bowl |
| Wrapping | Tyvek®/PET film pouch |
| Number of Wrapping Layers | 2 Layers |
| Closure Method | Heat Seal |
| Testing Method of sample | Immersion |
| Sterilization Cycle | Hard goods |
| Bag/Pouch Size | Double wrapped in a pouch with a larger outer bag |
Table 1: Examples of variables in a sterile hold time test
The movement of parts through the facility should be evaluated. Parts should be prepared and wrapped in such a way to facilitate material transfer. How the transfer process occurs post sterilization within a material handling airlock can have a major impact on the wrapping integrity which then can impact the microbial barrier of the wrapping. For example, surface sanitization of the wrapping or removal of an outer layer of wrapping should be tested and validated. The process of material transfer then allows for the sterile wrapped parts to be placed within the controlled cleanroom area. The final configurations of the wrapping after material transfer into a clean area is the wrapping that is tested for the sterile hold time.
Parts and equipment chosen during a study will determine the wrapping configurations to be tested. Wrapping material should be low particulate generating to limit the risk to the drug product. It also needs to be compatible with transfer methods into an aseptic area. Transfer is typically completed by application of disinfectants or alcohols onto the wrapped item prior to transfer from lesser classifications to the more critical areas. Once in the higher classifications, shedding the outer layer of wrapping material, if double wrapped, can be a faster and more streamlined material transfer method.
The wrapping of parts is decided based on the process and the aseptic presentation during use of the part, as the unwrapping of the part post sterilization is the highest risk for sterile surface contamination. Ease of unwrapping at the time of use minimizes the risk of contamination from operators and the environment. This is why the wrapping system needs to be configured for each specific process and part.
Closure methods are to be tested within a sterile hold study. Best practice closures avoid materials that could generate particles such as cellulose-based materials (“blue wrap”) and autoclave tape within the aseptic area. According to Annex 1, Section 8.48, “Where materials, equipment, components and ancillary items are sterilised in sealed packaging or containers, the packaging should be qualified for minimizing the risk of particulate, microbial, endotoxin/pyrogen or chemical contamination, and for compatibility with the selected sterilisation method…” The best practice closure methods allow for removal of parts from the packaging with limited contact from personnel or tools that could result in contamination and present risk to the final product.
Elasticized covers are used as initial barriers for product contact surfaces but are not considered a full microbial barrier. They allow for extra protection when installing parts and equipment that are product contacting to limit contamination by personnel handling during installation and line set up.
The time frame of the study is dependent on end-user processing restrictions and parts. For example, for complicated filling processes, 30-days hold time might be required for flexibility, while simpler processes might only need 7-days as the parts may be used quickly. Replications at the same timepoint are tested for repeatability. Multiple time points can be tested to increase confidence in longer sterile hold times.
Methodology
A study was conducted using parts, wrapping materials and closure methods shown in Table 2.
| Types of Wrapping and Closure Methods Used | ||||||
| Parts | Wrapping Material | Heat Seal | Self Seal | Gooseneck | Drawstring | Elasticized Cover |
| Stopper Bowl | All-Tyvek® Bag | N/A | N/A | X | N/A | X |
| Filling needle with Tubing (2) | All-Tyvek® Bag and Tyvek®/PET film pouch | N/A | X | N/A | X | N/A |
| Filling needle with Tubing (1) | Needle Bag with All-Tyvek® Bag | X | N/A | N/A | X | N/A |
| Glass Beaker | All-Tyvek® Bag | N/A | N/A | X | N/A | X |
| Stainless Steel Fitting | Tyvek®/PET film pouch | N/A | X | N/A | N/A | X |
| Forceps | Tyvek®/PET film pouch | N/A | X | N/A | N/A | N/A |
| Biological Indicators and Coupons | ||||||
| 1 | Tyvek®/PET film pouch | N/A | X | N/A | N/A | N/A |
| 2 | Tyvek®/PET film pouch | X | N/A | N/A | N/A | N/A |
| 3 | Tyvek®/HDPE film pouch | X | N/A | N/A | N/A | N/A |
| 4 | All-Tyvek® Bag- Needle Bag | N/A | N/A | N/A | X | N/A |
| 5 | All-Tyvek® Bag | N/A | N/A | X | N/A | N/A |
| 6 | All-Tyvek® Bag- Rigid Tyvek® | X | N/A | N/A | N/A | N/A |
| 7 | All-Tyvek® Bag- Needle Bag and Tyvek®/PET film pouch | N/A | X | N/A | X | N/A |
| 8 | All-Tyvek® Bag | X | N/A | N/A | N/A | N/A |
Table 2: Parts, Wrapping and Closure methods used during study.
To start the study, representative parts were chosen based on frequently used items in pharmaceutical aseptic fill/finish processing. Worst-case items were also selected based on size. i.e., the largest, bulky objects and the small, sharp objects that prove difficult to wrap. The parts tested were a stopper bowl, stainless steel fittings, tubing, filling needles, forceps and glass beakers. These parts were wrapped in best practice wrapping8 solutions listed above in table 2.
The closure methods, as shown in Table 2, were implemented based on the wrapping material used. All closures tested are the standard recommendations for each style of wrapping used. In addition to using representative parts, stainless steel and glass coupons were tested to minimize testing variability and ensure consistency. Using the coupons allowed for full immersion testing in a growth media.
A duration of 30-days was tested as a general duration for this evaluation, with sterility testing done at 10, 20, and 30 days. The timepoints of the study were in 10-day increments, allowing for more data to be collected for each wrapping configuration in the event of a failure at the longest time point of 30 days. The larger materials and representative parts were only tested at the 30-day mark with passing results.
During the testing period, one positive control for each time point tested was placed in the uncontrolled storage area with the wrapped and sterilized parts. Stainless steel coupons were wrapped in eight configurations (Table 2) with different closure methods and immersed in tryptic soy broth (TSB) for fourteen days to test sterility per USP 43 < 71>6. Table 3, below, lays out the number of samples tested at each time frame.
| Test Timeframe | Number of Samples | Types of Samples |
| Day 0 | 8 | Biological Indicators |
| Day 10 | 9 | Coupons (8), Positive Control (1) |
| Day 20 | 24 | Coupons (23), Positive Control (1) |
| Day 30 | 31 | Coupons (17), Positive Control (1), Representative Parts (13) |
Table 3: Number of samples sterility tested at each timepoint.
Results
See Table 4 for results summary.
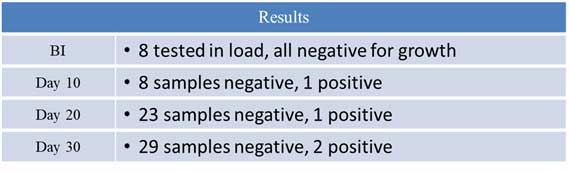
Table 4: Results from Sterile Hold Time testing
The results that were collected during this study showed data that was expected. The eight biological indicators were negative for growth, confirming that the sterilization cycle run on the parts was successful. The positive samples for each of the time points were the positive controls. The second positive sample at the day 30 time point was for a sample that was in a small, All-Tyvek bag without a positive closure, only a drawstring. This shows the importance of a positive closure to ensure the microbial barrier is intact. This data confirms a gooseneck closure (tortuous path) is required for a drawstring bag to maintain sterility of the contents.
Conclusion
Completing a hold time study maximizes the sterility assurance of your parts and equipment as well as the finished drug product. It also helps to reduce the reprocessing of sterile parts and equipment. This testing allows end users to store sterilized parts and equipment within the clean area to limit the amount of sterilization required on the day of processing. Parts tested and wrapping configurations should mimic routine wrapping practices. Justification can be used to limit the number of parts that are required to be tested using a risk-based approach. The testing summarized here supports a 30-day sterile hold time using Tyvek® bags, pouches and covers and can be used to aid in the design of a study protocol by the end-user, as well as to provide confidence in the package integrity time frame. Compliance with industry regulations is the responsibility of the end user / manufacturer, using their unique circumstances.
References
- European Union Guidelines. The Rules Governing Medicinal Products in the European Union. Volume 4 EU Guidelines for Good Manufacturing Practice for Medicinal Products for Human and Veterinary Use. 2022.
- United States Pharmacopeia 41 Chapter <1211>, “Sterility Assurance.” 2020.
- US Food and Drug Administration. “Guidance for Industry. Sterile Drug Products Produced by Aseptic Processing- Current Good Manufacturing Practice.” September 2004
- “Validation of Aseptic Processes- Using Media Fill” By Richard Chai and David J. W. Barber. Pharmaceutical Engineering March/April 2022.
- PDA Technical Report #22. “Process Simulation for Aseptically Filled Products.” Revised 2011.
- United States Pharmacopeia Chapter <71>, “Sterility Testing.” 2015.
- Poster Presentation. “Maximizing Sterility Assurance- Sterile Hold Time Testing for Autoclaved Items within Parenteral Drug Manufacturing.” PDA Microbiology Conference, October 10-11, 2022. Washington, DC. Renee Buthe.
- Technical Tip #0002. “Recommended Methods for closure of sterilization wrapping systems.” Revised 2018. STERIS reference 455-200-0002.
Renee Buthe Biography
Renee Buthe has been a member of STERIS Life Sciences Contamination Control Solutions as Technical Services Specialist since October 2021. In this role, Renee has responsibility for providing global technical support primarily for Sterility Assurance (i.e. biological and chemical indicators) and Barrier Products (i.e. sterilization wrapping), application and validation.
For 5 years, Renee has held positions within the Pharmaceutical Industry, specializing in environmental monitoring, sterility assurance, disinfection, sterilization and contamination control in parenteral drug manufacturing.
Renee holds a bachelor’s degree in Biology with a minor in Animal Sciences from the University of Kentucky.



















